<Title:> Brain machine Interface (BMI)-based Neurorehabilitation for Post-stroke Upper Limb Paralysis
<Author(s):> Meigen Liu, Junichi Ushiba
<Corresponding author E-Mill:> meigenliukeio(at)mac.com
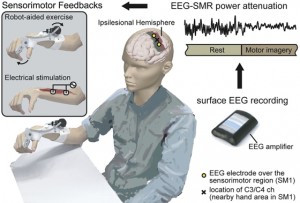
<Abstract:> Because recovery from upper limb paralysis after stroke is challenging, compensatory approaches have been the main focus of upper limb rehabilitation. However, based on fundamental and clinical research indicating that the brain has a far greater potential for plastic change than previously thought, functional restorative approaches have become increasingly common. Among such interventions, constraint-induced movement therapy, task-specific training, robotic therapy, neuromuscular electrical stimulation (NMES), mental practice, mirror therapy, and bilateral arm training are recommended in recently published stroke guidelines. For severe upper limb paralysis, however, no effective therapy has yet been established. Against this background, there is growing interest in applying brain machine interface (BMI) technologies to upper limb rehabilitation. Increasing numbers of randomized controlled trials have demonstrated the effectiveness of BMI neurorehabilitation, and several meta-analyses have shown medium to large effect sizes with BMI therapy. Subgroup analyses indicate higher intervention effects in the subacute group than the chronic group, when using movement attempts as the BMI-training trigger task rather than using motor imagery, and using NMES as the external device compared with using other devices. The Keio BMI team has developed an electroencephalography-based neurorehabilitation system and has published clinical and basic studies demonstrating its effectiveness and neurophysiological mechanisms. For its wider clinical application, the positioning of BMI therapy in upper limb rehabilitation needs to be clarified, BMI needs to be commercialized as an easy-to-use and cost-effective medical device, and training systems for rehabilitation professionals need to be developed. A technological breakthrough enabling selective modulation of neural circuits is also needed.
<Keywords:> electroencephalography, neurofeedback, mental practice, hand function, neuroplasticity
<URL:> https://www.jstage.jst.go.jp/article/kjm/71/4/71_2022-0002-OA/_html

![Incidence, Clinical Characteristics, and Long-term Outcome of the Dilated Phase of Hypertrophic Cardiomyopathy [Published online Keio J Med, 68, 87-94, by J-STAGE]](http://kjm.pupu.jp/blog/wp-content/uploads/2019/12/2018-0004-OA-100x100.jpg)
![Brain machine Interface (BMI)-based Neurorehabilitation for Post-stroke Upper Limb Paralysis [Published online in advanced , by J-STAGE]](http://kjm.pupu.jp/blog/wp-content/uploads/2022/06/2022-0002-OA-100x100.jpg)
![HIF Inhibition Therapy in Ocular Diseases [Published online Keio J Med, 71, 1-12, by J-STAGE]](http://kjm.pupu.jp/blog/wp-content/uploads/2022/03/2021-0004-IR-100x100.jpg)
![Current Management of Chronic Constipation in Japan [Published online Keio J Med, 72, 95-101, by J-STAGE]](http://kjm.pupu.jp/blog/wp-content/uploads/2023/12/2022-0036-IR-100x100.jpg)
![A Theory of Diagnostic Testing to Stop the Virus Spreading: Evidence-based Reasoning to Resolve the COVID-19 Crisis by Testing [Published online Keio J Med, 71, 13-20, by J-STAGE]](http://kjm.pupu.jp/blog/wp-content/uploads/2022/03/2021-0009-IR-100x100.jpg)
![Stroke and the Cell Therapy Saga: Towards a Safe, Swift and Efficient Utilization of cells [Published online Keio J Med, 66, 55-55, by J-STAGE]](http://kjm.pupu.jp/blog/wp-content/uploads/2017/09/66-005-ABST-100x100.jpg)
![Serum Neurogranin Measurement as a Biomarker of Central Nervous System Infections: A Preliminary Study [Published online Keio J Med, 71, 62-67, by J-STAGE]](http://kjm.pupu.jp/blog/wp-content/uploads/2022/09/2021-0019-OA-100x100.jpg)
![Diagnostic Performance of Computed Tomography Imaging for COVID-19 in a Region with Low Disease Prevalence [Published online Keio J Med, 71, 21-30, by J-STAGE]](http://kjm.pupu.jp/blog/wp-content/uploads/2022/03/2021-0012-OA-100x100.jpg)
![Activities of the Research Group for Comprehensive Research of Gene Mutation-related Rare and Intractable Diseases of the Skin within the Project for Research on Intractable Diseases of the Ministry of Health, Labor, and Welfare of Japan [Published online in advanced , by J-STAGE]](http://kjm.pupu.jp/blog/wp-content/uploads/2024/12/2024-0016-IR-100x100.jpg)
![Headache Caused by Brain Metastases of Castration-resistant Prostate Cancer during Cabazitaxel Therapy [Published online Keio J Med, 66, 65-71, by J-STAGE]](http://kjm.pupu.jp/blog/wp-content/uploads/2017/12/2016-0014-CR-100x100.jpg)